With each dollar of its grants, the National Institutes of Health — the world’s largest funder of biomedical research — generates, on average, $2.56 worth of economic activity across all 50 states.
The awards yield new drugs, like the naloxone spray used to prevent opioid overdoses, and breakthroughs in basic science, like the link between cholesterol and heart health.
But NIH grants also support more than 400,000 U.S. jobs, and have been a central force in establishing the country’s dominance in medical research. A recent survey by Nature found that, in health sciences, American research output is larger than that of the next 10 leading countries combined.
And that’s in large part due to federal government support of research conducted by universities. According to data from the Organisation for Economic Co-operation and Development, over the course of the past three decades, those universities have become, as a sector, the largest hub of nonbusiness research in the world.
Waves of grant terminations under the second Trump administration have thrown that relationship into doubt — and posed particular threats to certain kinds of research. Harvard has challenged the terminations in federal court. And in July officials confirmed they will provide 80 percent of expected expenses so that most defunded research inside the University can continue temporarily.
But that doesn’t protect researchers from the anxiety that comes with what could be a life-altering jolt. Another concern is lost time. Most of the affected grants support projects that touch many human lives. Disruptions have consequences.
Walter Willett, the Fredrick John Stare Professor of Epidemiology and Nutrition and — by one count — Harvard’s single most-cited scholar, worries about the maintenance of biobanks whose samples can date back 45 years.
The longitudinal studies behind these samples, including research conducted at Harvard and in Washington, generate insights by following populations over long periods of time. So an ill-timed loss of funding can leave an irremediable gap in the dataset or a question mark in place of a finding.
As his grants dried up in May, Willett and his team started “scrambling to try to protect the samples and the data we have”: freezers full of blood samples, DNA, and other biological material. Willett confirmed that those samples are safe this summer, thanks to the University’s stopgap funding. “But we still don’t have long-term solutions,” he added.
Of her four canceled grants, Molly Franke, an epidemiologist and professor of global health and social medicine at Harvard Medical School, worried most about a five-year randomized trial following roughly 160 teens and young adults living with HIV in Peru. The study tests a community-based support intervention that includes mental health support and healthcare liaisons who help them sign up for insurance, get government IDs, and enter treatment.
After the grant was canceled, that network of support was at risk of disappearing. “It was devastating,” she said. “These young people are often in very precarious social situations: Sometimes they don’t have adults in their lives; they’re struggling with mental health issues, substance abuse, or extreme poverty.”
Once University administrators committed to maintaining funding on a temporary basis, researchers breathed a small sigh of relief.
But Franke will still have to look for other backers to make sure the Peru study can be brought to a satisfactory conclusion. Her team tries to lighten the toll of disease in far-flung places because they believe “it’s the right thing to do,” she said. But the work is far from irrelevant to Americans, she noted.
“Infectious diseases know no borders,” Franke said. “And when we get drug-resistant tuberculosis in this country, we know how to treat it because of studies conducted elsewhere.”
In the spring of 2024, Kelsey Tyssowski — a research associate in organismic and evolutionary biology — received a grant of $130,255 through the NIH’s BRAIN Initiative for her work on the nervous systems of deer mice, in the hopes that it might shed light on ALS and other neurodegenerative disorders. (That may sound like a stretch, Tyssowski acknowledged, before pointing out that “skilled movement is the thing that people lose first with a lot of diseases.”)
But, as with nearly all other government grants to Harvard, those funds were finally revoked in early May.
Across 15 years in labs, Tyssowski said she’s been funded by government money “more often than not.” Her latest grant was supposed to serve as a bridge between her postdoc in the lab of Hopi Hoekstra and a tenure-track job, and a dedicated lab, probably on another campus.
“I may be the only person studying skilled movement, from this angle, right?” she said with a laugh. “I’d like to start my own lab, and train other people to do this. And if I can’t do that, all of the money and time and energy that’s gone into getting me to this point will have been almost completely wasted.”
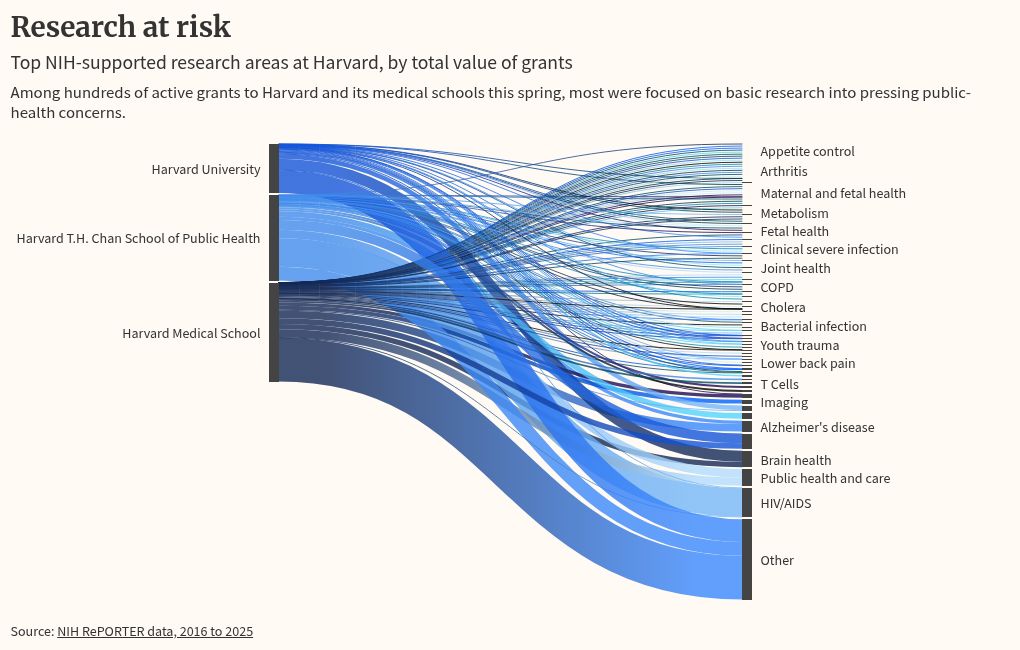
Similar stories are playing out across Greater Boston and elsewhere in the nation’s research hubs. Grant data from the NIH shows that affected researchers at Harvard were working across a variety of medical frontiers, from cancer immunotherapy and stem cells to environmental health.
But researchers also stress that their work is not limited to labs on campus or in local hospitals.
At Harvard Medical School, the termination of 350 grants — totaling $230 million in annual funding — has also entailed the cancellation of over 100 “sub-awards.” Those are funds that pass through to partner institutions — in Harvard’s case, in 23 states and Washington, D.C. — that might have better access to animal species or lab resources.
Jonathan Abraham, associate professor of microbiology at HMS, won a grant to analyze mosquitos en route to a better understanding of Eastern equine encephalitis, or EEE. And it came with a sub-award for the University of Texas Medical Branch, as the world’s largest depository of insect-borne viruses.
Meanwhile, Stephanie Mohr won a similar sub-award for a team at the University of Maryland School of Medicine, for a study of tick biology that hoped to shed light on Lyme disease. They were just a few months into a five-year grant when the termination hit.
The same goes for Franke’s study of HIV in youth, which involved a sub-award to the Peruvian branch of Partners In Health.
That study involved, she said, a commitment not just to patients but to the staff paid to care for them and to Peru’s Ministry of Health. The collapse of one grant had ripples of risk, even thousands of miles away.
“It affects the care, people’s livelihoods … and a trust that had taken 20 years to build,” Franke said. “That was what kept me up at night.”
Source link